Eliminating Preventable Harm
Patient safety advances at Johns Hopkins stretch back almost 150 years. Many of the programs and safety metrics developed here have been adopted worldwide.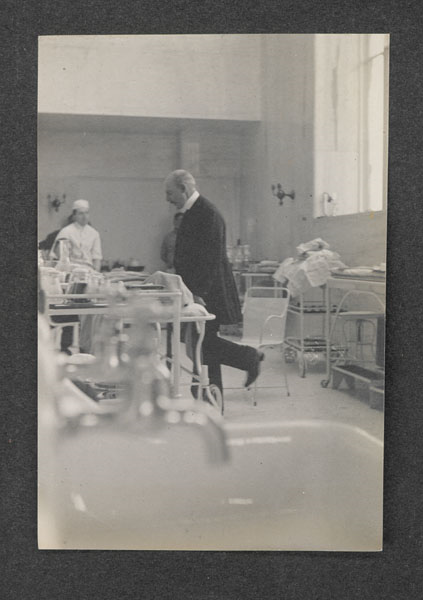
William Stewart Halsted, the first surgeon-in-chief at the Johns Hopkins Hospital, introduces the use of rubber gloves to the operating room.

Hopkins physician Hugh Hampton Young discovers the antiseptic properties of merbromin, best known by the brand name Mercurochrome.
Neurosurgeon Walter Dandy creates what many believe is the first post-operative intensive care unit (ICU).
Three-bed, 24-hour nursing unit serves critically ill neurosurgical patients.
Learn MoreJohns Hopkins establishes institutional review boards (IRBs) to protect the rights and welfare of human subjects in medical research.
The first three institutional review boards are for the School of Medicine, Bloomberg School of Public Health, and the Homewood campus.
Learn More
Ruth Faden, founding director of the Johns Hopkins Berman Institute for Bioethics, co-authors the first bioethics textbook: A History and Theory of Informed Consent.
Two preventable patient deaths lead to what some consider the most significant culture change in the history of Johns Hopkins Medicine as institutional leaders make patient safety JHM’s top priority.
"These events created a moral moment where we had to make a choice. It was: Are we openly going to address our shortcomings? Or are we going to hide behind our brand and say all is well? Leadership stood up and said, ‘We need to start talking about this.'"- Peter Pronovost Learn More

Peter Pronovost, Johns Hopkins critical care physician, publishes a five-step checklist that goes on to drastically reduce bloodstream infections.
With a $10 million gift, the Armstrong Institute for Patient Safety and Quality is established.
"A preventable harm mistake almost killed me. Thus, my passion today is never again—for anyone."- C. Michael Armstrong, founding donor and former board chairman for Johns Hopkins Medicine. Learn More

The first patient and family advisory councils help evaluate strategies and improve quality and safety outcomes.
The Armstrong Institute creates three centers of excellence.
They are designed to prioritize health care worker safety and patient outcomes.
Learn MoreLooking Forward
A new artificial intelligence system developed at Johns Hopkins catches symptoms of deadly sepsis hours earlier than traditional methods, potentially saving thousands of lives.
According to Johns Hopkins Magazine, patients are 20% less likely to die of sepsis because the system scours medical records and clinical notes to identify patients at risk of life-threatening complications. The work could significantly cut patient mortality from one of the top causes of hospital deaths worldwide.
“It is the first instance where AI is implemented at the bedside, used by thousands of providers, and where we’re seeing lives saved,” says Suchi Saria, founding research director of the Malone Center for Engineering in Healthcare at Johns Hopkins. Her studies, published in 2022 in Nature Medicine and Nature Digital Medicine, evaluated more than a half million patients over two years. “This is an extraordinary leap that will save thousands of sepsis patients annually.”

Credit: Will Kirk / JHU
Calls to Action

Join the Celebration
For 150 years, we’ve been breaking new ground—now, let’s celebrate it. Join us for gatherings, lectures, and special events that honor our legacy and look ahead. Details on future events are coming soon.
Learn more
Hopkins Retrospective
Hopkins Retrospective is an initiative designed to expand our understanding of the diverse history of Hopkins and weave that history into the university experience.
Learn more


